Environmental Hygiene: The Critical Link to Patient Safety and reduction of HAIs

Environmental Hygiene is foundational to infection prevention, yet Environmental Services (EVS) professionals remain undervalued and under-resourced. As healthcare systems face financial pressures, EVS departments are often targeted for cuts—an alarming trend that increases patient risk and shifts cleaning responsibilities to nurses already overwhelmed with clinical care.
EVS Cuts Increase Risk
I will never forget the conversation I had with an ED nurse of a large Children Hospital. She explained that during cold and flu season, all they have time to do is wipe off the gurney rails and turn over the sheets before bringing in the next patient. While nurses should receive some basic cleaning and disinfection training, expecting them to manage both clinical care and effective cleaning and disinfection—because EVS is allotted only ten minutes per room per day—is unrealistic and unsafe. Let’s put it this way: consistent and effective cleaning and disinfection is not happening. This leads to higher rates of healthcare-associated infections (HAIs), staff burnout, and poorer outcomes.
Training Gap
EVS professionals are the first line of defense in infection prevention, yet foundational and ongoing training is too often viewed as non-essential. This is a dangerous misconception. Healthcare cleaning and disinfection is a specialized discipline—one that must account for high-traffic, high-contamination environments, immune-compromised patients, and complex medical equipment requiring specific disinfectants and protocols. Add to that the invisible world of pathogens that must be eliminated to prevent healthcare-associated infections (HAIs), and the need for specialized training becomes undeniable.
A 2022 study published in Antimicrobial Stewardship & Healthcare Epidemiology demonstrated that implementing formal EVS education, monitoring, and feedback systems led to sustained cleaning performance above 90% and a 75% reduction in Clostridium difficile infections over a 10-year period [1]. Similarly, the CDC’s EVS and the Battle Against Infection training program emphasizes that EVS personnel play a critical role in preventing HAIs by following evidence-based cleaning and disinfection protocols[2].
Moreover, healthcare is a highly regulated industry under constant scrutiny. Facilities must comply with State, Federal, CDC, OSHA, and Joint Commission standards. Training is not a luxury—it is a regulatory and ethical imperative.
It is a sad but familiar truth: everyone knows someone who has acquired an infection while being treated for something unrelated. This is not a distant issue. Investing in EVS education ensures these professionals are equipped to protect patients, staff, and themselves—while also safeguarding the reputation and compliance of the healthcare facility.
The Myths of “Quick Cleaning,” “High-Touch Focus,” and “Self-Cleaning Surfaces”
A growing body of research challenges the notion that quick surface wiping is sufficient. Studies show that improper wiping techniques—such as using the same cloth across multiple surfaces—can spread contamination rather than eliminate it. In a study led by Dr. Syed Sattar, using the ASTM E2967-15 standard, researchers found that while several disinfectant wipes reduced microbial load, only one product—containing 0.5% accelerated hydrogen peroxide—prevented the transfer of pathogens like Staphylococcus aureus and Acinetobacter baumannii to clean surfaces [3].
The “one wipe, one surface, one direction, dispose” method is now recognized as best practice, yet it is rarely enforced due to time constraints and lack of training. Focusing solely on high-touch surfaces while neglecting others creates blind spots in infection control and fosters a false sense of security.

Further supporting this, a 2022 study published by Oxford Press evaluated wipe-based decontamination methods and found that certain disinfectant wipes, when misused, contributed to increased microbial transfer rather than reduction[4]. These findings underscore the critical need for proper technique, product selection, and training.
Focusing solely on high-touch areas while neglecting others creates blind spots in infection control. As of the writing of this blog, I still have not been able to define what high touch surfaces are. To truly understand this, one must observe the behavior of healthcare professionals—whether they are nurses, certified nursing assistants, medical or lab techs, family or visitors as well as the patient. By doing this, you quickly begin to realize there is no such thing as high-touch versus highly-touched surfaces. True environmental hygiene requires a comprehensive, evidence-based approach—not shortcuts.
The topic of antimicrobial surfaces deserves its own dedicated discussion, but one point is essential here: there is no such thing as a completely “self-cleaning” surface. Antimicrobial materials can help reduce bioburden, making surfaces easier to clean effectively, but they do not replace the need for thorough cleaning and disinfection. Without regular cleaning, contaminants can still build up and even interfere with the surface’s antimicrobial properties. Every surface, regardless of its material, must be properly cleaned and disinfected to support infection prevention.
Room Turnover Needs Time
Hospitals often demand room turnover in 10–15 minutes, but effective terminal cleaning takes 40–45 minutes. Rushing this process undermines infection prevention and devalues EVS expertise. Cleaning is a process-driven discipline—shortcuts are dangerous.
Call to Action
To protect patients and support healthcare workers, we must:
- Increase EVS staffing, especially in high-turnover areas like Emergency Departments
- Require foundational and ongoing training and certification
- Require basic foundational cleaning and disinfection training for all staff responsible for patient care
- Evaluate and address room turnover time requirements to support patient safety and care
- Implement evidence-based cleaning protocols
- Consider the cleaning and disinfection requirements of any given environment and select surfaces and products that support effective cleaning and disinfection without causing damage.
Environmental hygiene is not a cost center—it’s a strategic asset. Patient safety depends on it.
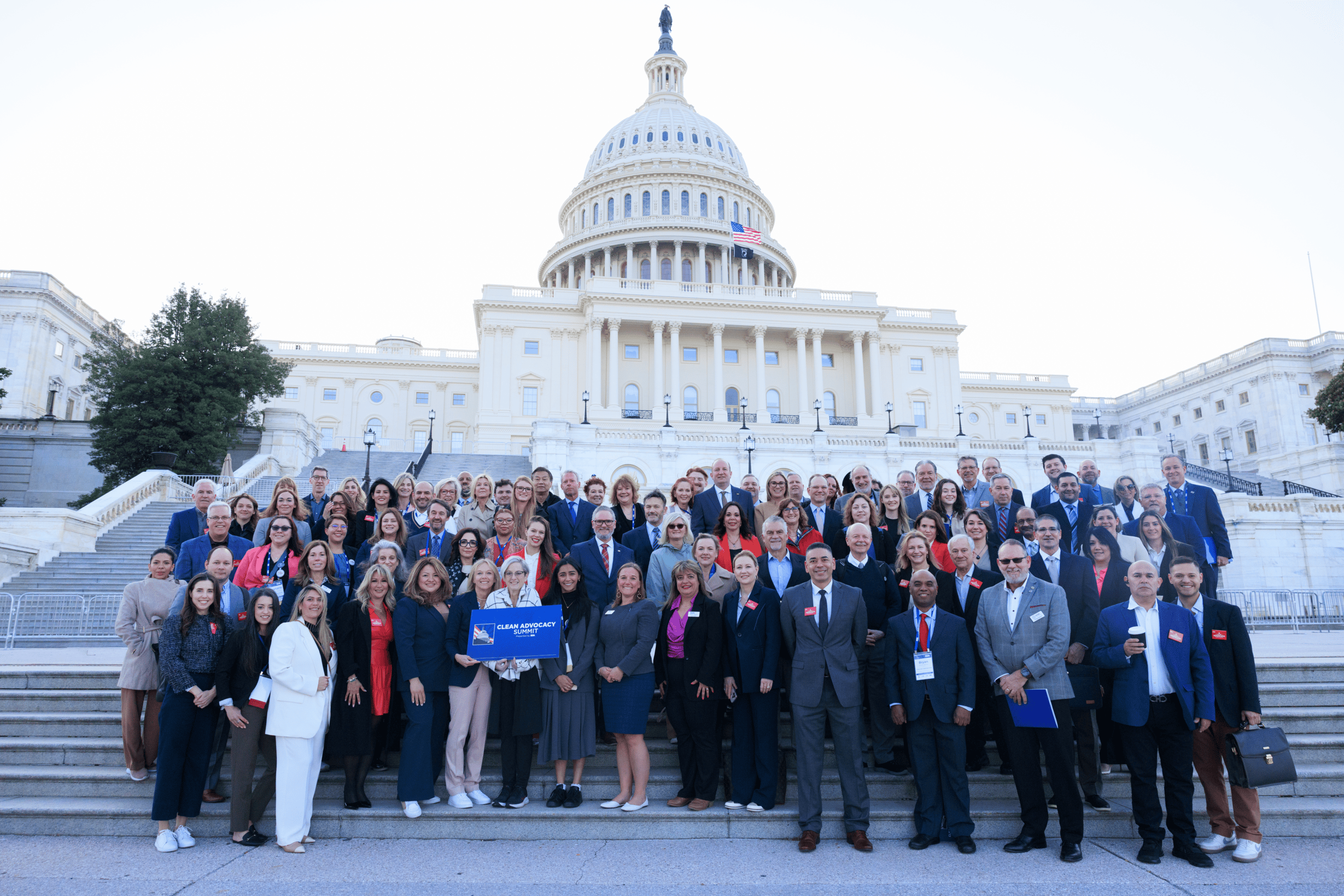
ISSA Healthcare is launching soon: the new platform will equip professionals with the training, guidance, collaboration, and support needed to support safe, hygienic healthcare environments. Join the interest list now to get updates at issa.com/healthcare.
References
[1] Environmental cleaning and disinfection: Sustaining changed practice … [2] Training: EVS and the Battle Against Infection | Infection Control | CDC [3] Disinfectant wipes are appropriate to control microbial bioburden from … [4] Preventing Viral Contamination: Effects of Wipe and … – Oxford Academic