Global HAI Data 2025: Trends, Risks, and the Role of Training

Introduction
Healthcare-associated infections (HAIs) remain one of the greatest ongoing challenges in healthcare, drastically impacting patient safety, recovery, and hospital resources worldwide. Despite advances in medicine, the latest World Health Organization (WHO) report underscores a persistent truth: nearly 1 in 10 patients will acquire an HAI during their care. These infections not only prolong hospital stays but also drive up costs, increase morbidity, and—most alarmingly—contribute to preventable deaths. Preventing HAIs demands continual vigilance, and dedicated healthcare education and certification programs are more essential than ever for equipping professionals with the latest skills and strategies.

Global HAI Statistics: A Stark Picture
The WHO’s most recent figures show the following trends:
- Globally, about 10% of patients suffer an HAI while receiving health services.
- In high-income countries, 7 out of 100 hospital patients will contract at least one HAI; this risk increases to 15 in 100 in lower-income regions, often due to resource limitations and less robust infection prevention systems.
- Intensive care units experience even higher prevalence, with rates as high as 30%, particularly in hospitals without rigorous infection control support.
- Antimicrobial resistance (AMR) is compounding the issue. AMR-related HAIs now total an estimated 136 million cases each year, with the highest burden carried by middle-income countries.
These statistics translate to millions of extra hospital days and significant financial cost—the WHO notes that in Europe alone, patients collectively spend 25 million additional days in the hospital each year because of HAIs. The costs add up to billions annually, straining health systems and impacting patient outcomes.
The Threat of Antimicrobial Resistance
Alarmingly, the growing force of antimicrobial resistance is intertwined with the HAI crisis. More than 5 million deaths each year are now linked to AMR, and healthcare settings are a primary source of resistant infections. For patients, contracting an HAI caused by resistant bacteria means longer recovery, higher chances of complications, and—in many cases—a significantly higher risk of mortality. The increased threat makes the case even stronger for comprehensive training and adherence to best practices in infection prevention.
Pandemic Effects and the HAI Landscape
The COVID-19 pandemic exposed weaknesses in infection prevention, disrupting established routines, straining supplies, and increasing the rate of healthcare-associated infections globally. Throughout the pandemic, many facilities faced organizational challenges and staffing constraints that affected infection control programs, leading to substantial increases in HAIs—especially central line-associated bloodstream infections, catheter-associated urinary tract infections, ventilator-associated events, and MRSA bacteremia. As healthcare emerged from the pandemic, it became clear that investment in ongoing education and certification for infection prevention is critical for greater resilience and improved outcomes moving forward.
Best Practices for Preventing HAIs
Solving the HAI problem requires more than awareness—it needs reliable systems, evidence-based practice, and consistent staff engagement. WHO and other global leaders recommend, in addition to other recommendations, a core set of interventions:
- Mandatory hand hygiene education, supported by WHO’s global hygiene campaign and regular compliance checks.
- Proper use, maintenance, and timely replacement of invasive devices (catheters, IV lines, ventilators).
- Routine, standardized cleaning and disinfection protocols, including targeted attention to high-touch surfaces.
- Emphasis on antimicrobial stewardship to slow the spread of resistant organisms.
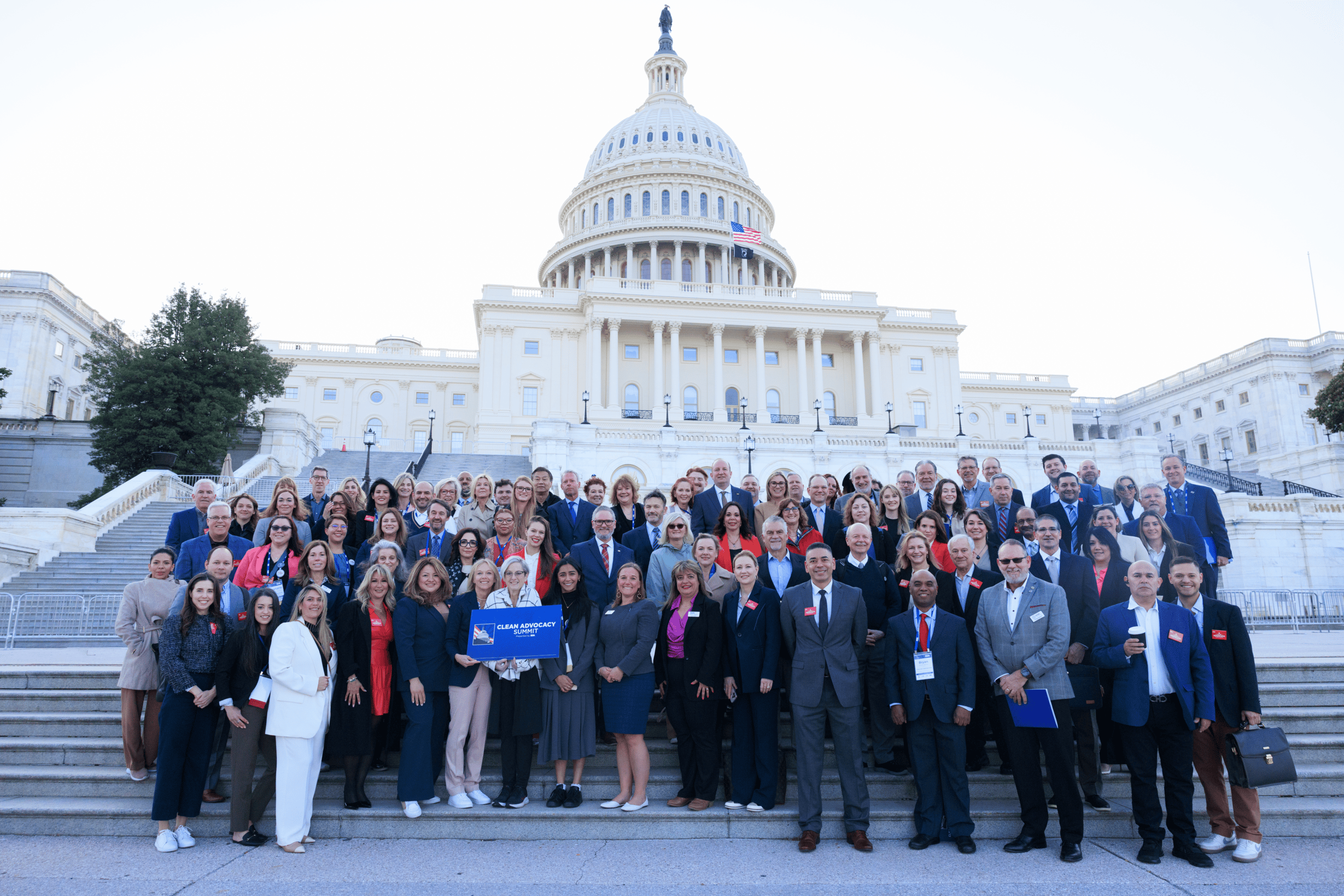
To reduce transmission, healthcare organizations should invest in regular training and certifications, creating a culture of safety and accountability.
Surfaces: The Overlooked HAI Vector
Surfaces in patient rooms, operating theaters, and even waiting areas act as silent transmitters of infections. Research highlighted by the Healthcare Surfaces Institute shows that improvements in cleaning methods, material choices, and surface design contribute significantly to lowering HAI risk. Facilities that combine environmental cleaning protocols with ongoing staff training report fewer outbreaks and safer environments for both patients and staff.
Conclusion
The toll of healthcare-associated infections—from human suffering to system-wide costs—is too great to ignore. The latest data from the WHO emphasizes that coordinated action, from frontline education to environmental management, is essential for progress. By staying informed, investing in robust training, and updating infection prevention strategies, healthcare organizations worldwide can make measurable advancements in patient safety and quality of care.