Floors, Frequency, and False Assumptions in Healthcare Cleaning
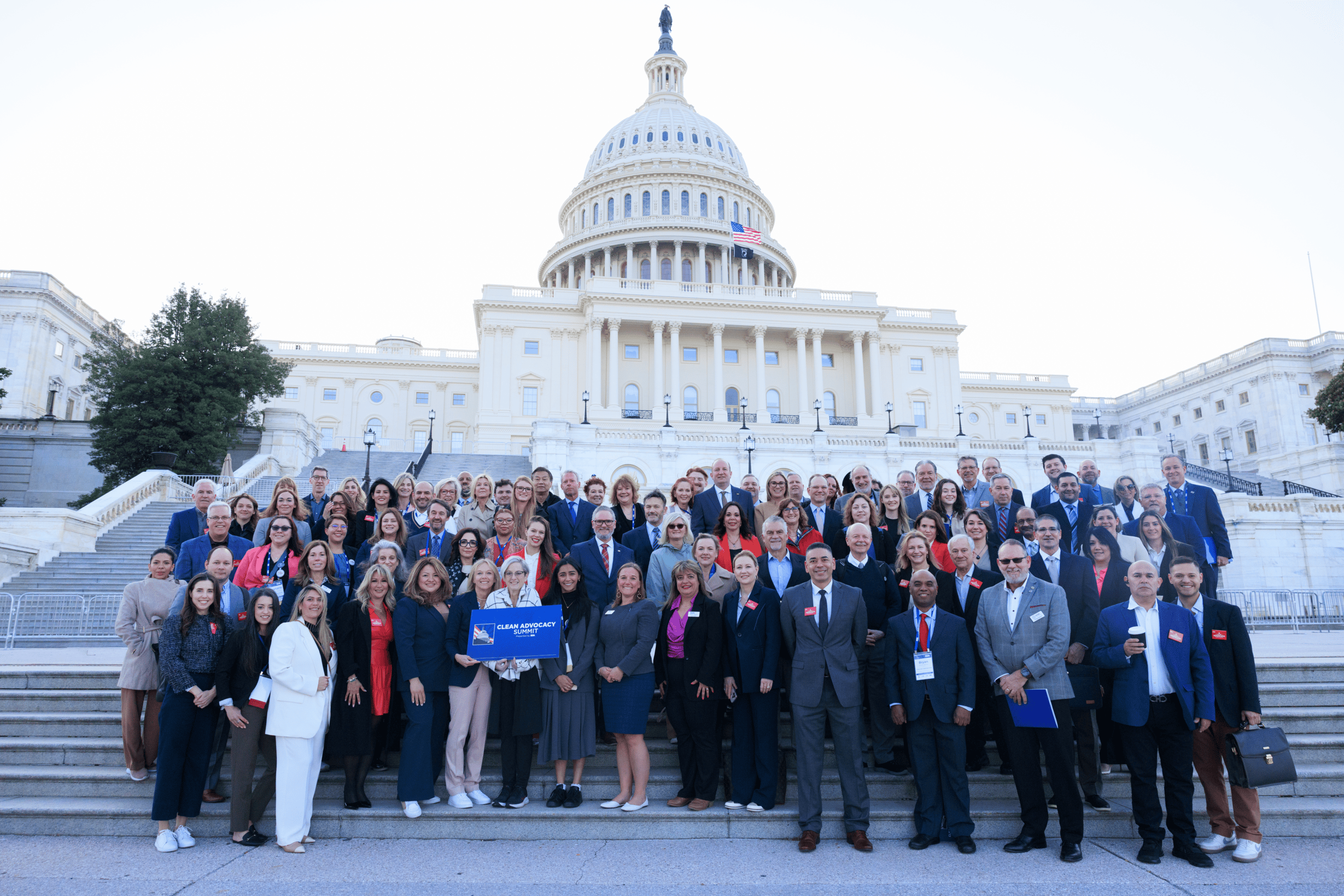
Floors are the surfaces everyone touches—just not with their hands. That’s the uncomfortable truth discussed in a recent ISSA Healthcare session led by Linda Lybert, executive director of the Healthcare Surfaces Institute, a division of ISSA, along with three floor-care experts: Keith Schneringer of BradyPLUS, Chris Farrell of Contec Professional, and Rich Feczko of Elevate Innovation Group.
Lybert shares a reality check that will sound familiar to anyone who has tried to prioritize floor care in a hospital: “Patients aren’t on the floor.” She explains that microbes don’t need patients lying on the floor to spread; they only need traffic, wheels, dust, and human behavior.
In the webinar, Lybert mentions a five-hospital study that swabbed floors for MRSA, VRE, and C. diff and found floors heavily contaminated—sometimes even more than the “high-touch” surfaces hospitals focus on. Whether the specific numbers surprise you or not, the implications are clear: If floors are frequently contaminated and connected to everything else in the room, then considering floors as low-risk is a dangerous assumption.
Where cross-contamination actually occurs
Once the panel begins identifying how microbes spread, the argument that “patients aren’t on the floor” quickly falls apart. Feczko points out the obvious sources: “Anything on wheels that’s going to travel,” including gurneys, IV poles, wheelchairs, and equipment moved from room to room. If those wheels aren’t cleaned and disinfected regularly, they become mobile transfer points.
Farrell highlights a subtle but important issue: the increase of personal electronics in the patient room. Phones, chargers, tablets, cords, and personal belongings constantly move in and out—from bed to chair to floor and back. Even in areas with strict protocols, these items are seldom cleaned as thoroughly as medical equipment.
Schneringer highlights another overlooked pathway: dust. Floor contamination isn’t just about footsteps; it’s also about “aerosolization and movement throughout rooms,” where particles can carry pathogens. In other words, the floor doesn’t stay on the floor.
Why floors don’t get cleaned more often: Lybert shares a blunt example. A colleague observed an emergency department for 12 hours and saw no floor cleaning unless there was a visible body fluid spill. In high-traffic areas like the ED, where patients, staff, equipment, and pathogens circulate nonstop, “clean when you see it” is not a strategy. It’s a limitation disguised as a routine.
The panel agrees that the obstacles are familiar: time, access, and outdated assumptions. Feczko explains that hospital floor care is still often based on frequency and square footage instead of the task itself, a legacy framework that doesn’t reflect what science and data are now showing healthcare leaders about contamination risk.
Schneringer explains it in operational terms: environmental services teams have a limited window to complete multiple priorities, and floors have traditionally been considered “not a high touch surface.” When the checklist is full, the “invisible” work is the first to be sacrificed.
And yet, “invisible” is exactly what floors are—until a survey, an outbreak, a complaint, or a leadership walkthrough.
The perception issue (and why it persists): If you want a quick way to grab leadership’s attention, don’t focus on bacteria counts. Begin with what patients observe.
The panel often returns to perception—especially since HCAHPS scores influence how facilities are evaluated. Feczko mentions that many surveys reward perception over actual conditions, but he also warns that perception can quickly lead to actions. A dirty-looking floor, stained curtains, or a questionable mop bucket in a highly visible corridor can create an impression that doesn’t go away just because the rest of the room is clinically compliant.
Farrell goes further with an ED-centric point: emergency rooms are ripe for process improvement. They’re high-volume, high-traffic, and often the first place a patient forms an opinion about the facility’s safety and competence.
Cleaning must be designed into the building
One of the most pointed discussions centers on the root issue many EVS leaders already feel: they’re asked to achieve clinical outcomes in spaces that were never intended for that purpose maintained.
Feczko emphasizes that environmental services must be involved in decisions about “flooring types” and flooring placement. Too often, floors are chosen for their appearance—what Farrell calls a “focus on form rather than function”—with little consideration of how those materials perform during actual cleaning cycles, with real chemistry, and under real labor conditions.
Schneringer highlights the on-the-ground frustration of transitions: a tech might move from LVT to VCT to terrazzo to marble in a single zone. This creates training complexity, chemical compatibility risks, and more chances for mistakes. Farrell adds an example that will sound painfully familiar: when results aren’t good, teams default to “more is better,” adding more chemical and leaving sticky residue that makes floors look worse and attracts more soil.
In other words, choosing the wrong floors doesn’t just cause cleaning issues. They also lead to recurring problems—affecting appearance, safety, cost, and workload—all at the same time.
Cleaning versus disinfection
When the discussion turns to disinfecting floors, the panel remains clear: first clean, then disinfect. Cleaning removes soil and bioburden through agitation. Disinfection requires dwell time to effectively do its job.
Feczko clearly states: “You can’t remove microbes or fomites or bacteria from a surface without agitation.” Disinfectants, he notes, require “functionality time.” Schneringer observes the post-pandemic “arms race” for quicker claims—five minutes, two minutes, one minute, even “15 seconds.” However, the panel’s concern remains the same: claims are irrelevant if the process cannot be properly carried out.
And execution, Farrell argues, is where many programs fail. He is careful not to blame EVS workers, saying failures are usually due to “tools, process, or training” problems—not lack of effort. If leadership wants better results, the solution is often not to demand more speed. It’s to create a better system.
The microfiber reality check
A memorable portion of the discussion dives into microfiber. The panel agrees microfiber is highly effective—until it isn’t. Farrell explains that microfiber can carry “bio burden” over time due to residues that accumulate through repeated laundering. The point isn’t that microfiber is bad; it’s that the industry often assumes “hygienically clean” always equals functionally clean for clinical outcomes.
The main takeaway is the same theme that runs throughout the session: if you don’t understand the interaction between tool, chemistry, and process, you can end up creating the problem you think you’re solving.
Technology helps, but it doesn’t replace manual cleaning. The panel discusses UV and HPV technology with a clear agreement: it’s only an addition. Feczko says, “There’s nothing that can replace manual cleaning.” UV isn’t removing soil; it’s enhancing disinfection after the cleaning is done.
Schneringer mentions practical constraints—UV requires empty rooms, and some surfaces may degrade with repeated exposure. However, the group remains optimistic about innovation overall, especially tools that help teams work more safely and consistently without adding time pressure that makes the process impossible.
What EVS pros can do right now
Lybert’s closing question is the one EVS professionals have asked for years: Where do we start?
The panel’s answer is not a single product or protocol. It’s alignment.
Begin with collaboration: EVS, infection prevention, nursing leadership, and facility decision-makers need a shared plan and clear ownership, “who owns what and who cleans what,” as Feczko describes it. Then, focus on high-risk areas—ED, sterile fields, burn units, isolation rooms—and update expectations for frequency and execution based on data, not tradition.
And perhaps most importantly, stop treating floors as the surface of last resort. Whether patients are “on the floor” or not, the floor still touches almost everything that touches them.
Stay informed on related topics at issa.com/healthcare