Passing the Baton: How to Combat the Recent Rise in HAIs

The increase in HAIs (healthcare-associated infections) during 2021-22 has raised concerns about patient safety in the most recent Leapfrog Hospital Safety Grade report. During this timeframe, there was an all-hands-on-deck focus on Covid 19 – caring for patients, assuring healthcare workers’ safety, and controlling the spread of the SARS-CoV-2 virus. Until then, efforts to identify HAI causes and enact solutions to prevent HAIs had been working, and HAIs were trending down. Unfortunately, when competing pressure from the Covid 19 pandemic disrupted established practices, the trend reversed.
The Healthcare Surfaces Institute has determined that one of the primary ways microbes move within a healthcare setting is via surfaces. Yet, most infection prevention strategies overlook surface safety issues beyond cleaning. Surfaces don’t just mean hard surfaces such as countertops, floors, and walls, but all parts of patient beds-rails, head/foot boards, reusable medical devices in patient care areas, as well as soft surfaces including mattresses, carpets, and textiles – window coverings, privacy curtains, and bed linens.
There are different protocols for cleaning hard and soft surfaces, but the same disinfectants or cleaning agents do not necessarily have indications for use on both. A careful reading of the IFU (instructions for use) for both the disinfectant and the surface to be disinfected before implementing procedures is key.
Complicating the cleaning and disinfecting of surfaces to kill or inactivate microorganisms is the presence of biofilms. Dr. Rodney E. Rhode, PhD, Texas State University’s Clinical Laboratory Science Regents’ Professor and Chair, described the phenomena of biofilm in a recent blog.
“A biofilm is a three-dimensional structure formed after microorganisms sense and adhere to surfaces, followed by subsequent colonization and production of an extracellular polysaccharides matrix (EPS).” He goes on to point out that “most human infections are likely biofilm mediated.”
By not properly cleaning and disinfecting inanimate surfaces, microorganisms can be transferred to patients where the conditions for biofilm exist and the cycle continues. It’s at the intersection of surfaces that we need to “mind the gap” where positive and negative charges and chemical interactions can create an unbalanced environment.
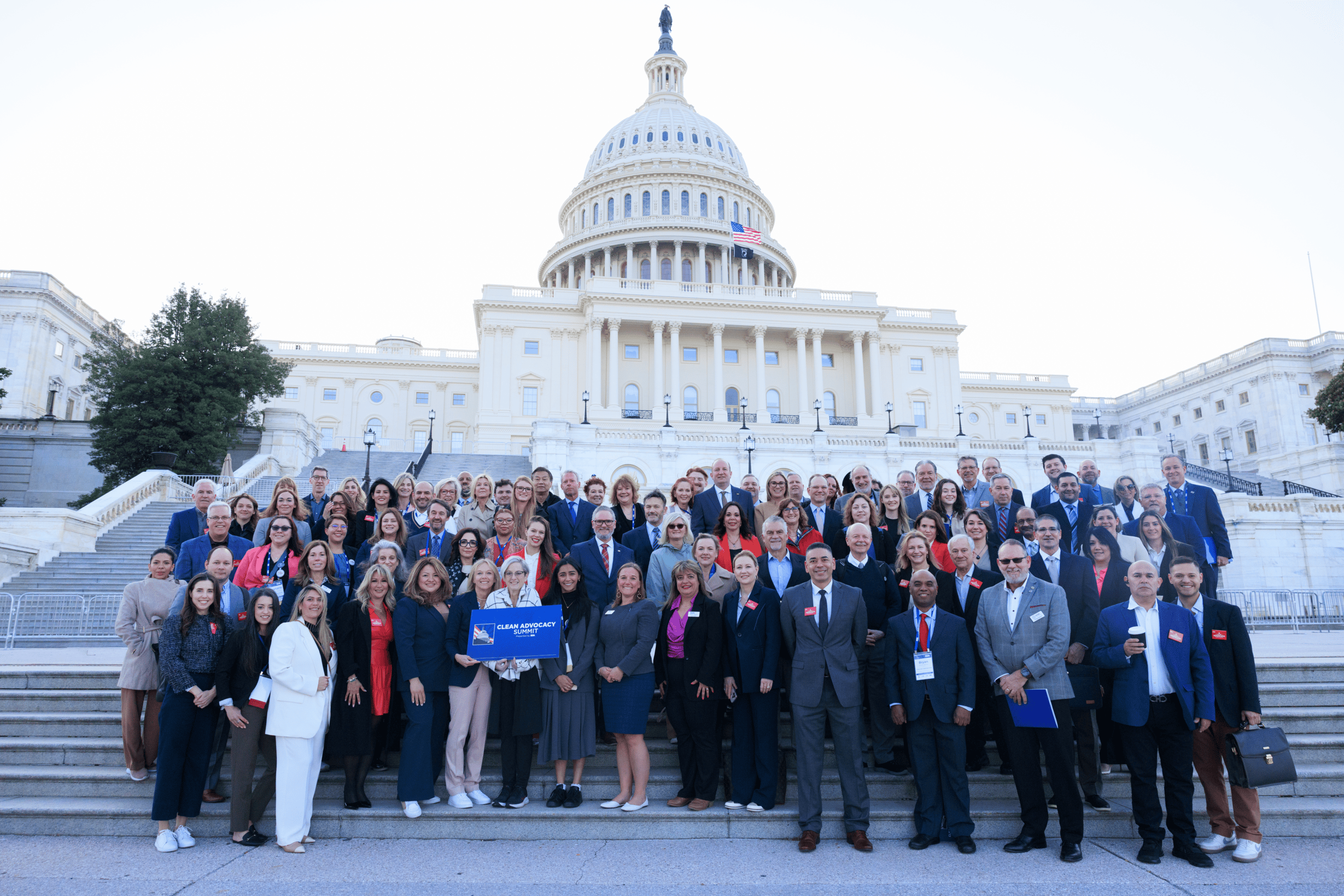
The key to controlling HAIs lies in education across the healthcare industry – from materials and medical device manufacturers and cleaning and disinfection chemists to EPA and FDA and other regulatory agencies to Infection Prevention & Control and Environmental Services professionals. This may be in the form of certifications, guidelines, revamping of IFUs, or recalibration of policies and practices. All entities must implement a handoff à la a relay race where the baton must remain in play and not be dropped, causing a disqualification in the race to eradicate HAIs.